Charting a New Course: Working Upstream to Address Social Determinants of Health
The significant impact of social factors on public health are well-known. Yet, the US healthcare system is only recently making strides to address this topic. In a recently published chapter in The Affordable Care Act as a National Experiment: Health Policy Innovations and Lessons (Selker, 2021), Dr. Sarah Bliss Matousek (Principal at Day Health) and colleague Niko Lehman-White discussed social determinants of health (SDOH) and began to explore ways that the healthcare system can affect positive change. Matousek and White outline the five major SDOH categories: economic stability, education, neighborhood and built environment, health and health care, social and community context, as illustrated below. For more detail on each, refer to the full book chapter.
Graphic content source: The US Office of Disease Prevention and Health Promotion, Healthy People Framework, 2020.
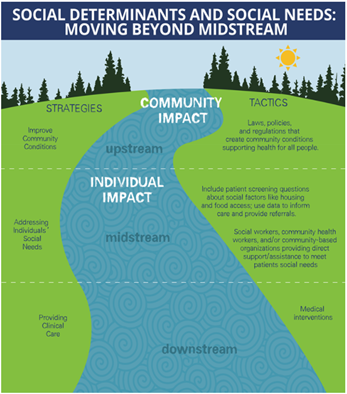
Yet, the full continuum of SDOH must be addressed to move the needle on health outcomes. To address the upstream SDOH, we must first identify and then scale successful interventions that address individual social risk factors and social needs.
Source: “Meeting Individual Social Needs Falls Short Of Addressing Social Determinants Of Health, " Health Affairs Blog, January 16, 2019. DOI: 10.1377/hblog20190115.234942
In their chapter, Matousek and White use Cuba’s approach to exemplify success in addressing individual social risk factors and social needs. Despite the vast differences in resources compared to the United States, Cuba has managed to redefine healthcare delivery through personalized medicine. Annual checkups, for example, take place at patients’ homes. This enables providers to honor and understand other factors that may impact the patient’s health, like their family life, home environment, social connections, and other social factors. Most importantly, the data shows that this approach is working through metrics such as low infant mortality rates and a higher life expectancy.
Addressing Social Needs in the United States:
Case Example of a Systematic Approach
Over the past decade, the healthcare provider system and state Medicaid agencies in the United States have come together to implement strategies that, like Cuba, prioritize addressing the full continuum of SDOH. The North Carolina Healthy Opportunities Pilot is one way a state is currently taking a systematic approach to addressing social needs. This program is centered around four priority areas of social needs: (1) housing, (2) food, (3) transportation, and (4) interpersonal safety services. Pilot services focus efforts on these priority domains through approved services such as one-time payments to secure housing, medically tailored meal deliveries, payment for public transit, and legal services for interpersonal violence, among many others.
Patient identification and eligibility are key to reaching the populations most in need of services. To qualify for pilot services, Medicaid managed care enrollees must meet at least one needs-based criteria and at least one social risk factor.
The health system is responsible for identifying needs-based criteria and screening for social risk factors, a task that can only be done through a person-centered approach to care. For example, a 60-year-old male may have developed diabetes, in addition to his existing hypertension, between office visits at a health system in North Carolina. While the doctor identifies and records the patient’s updated health status, the doctor also screens the patient for social risk factors by asking questions about housing status and levels of safety at home. It is during these conversations that health care professionals can go beyond traditional routine clinical care and achieve whole-person care. For example, if the man reveals that he is living in a shelter, the doctor can quickly identify that he meets the eligibility criteria to be eligible for pilot program services.
Conclusion
By identifying risk factors to address social needs, programs like North Carolina Healthy Opportunities Pilot can truly move the needle toward influencing the broader associated social determinants of health. Day Health has been working with ACO and state government clients to develop and refine model of care strategies specific to frameworks similar to that used by the North Carolina pilot program. We want to encourage more states and health systems to see the value and begin piloting this type of approach. We look forward to tracking evaluation outcomes and assisting healthcare systems with implementing best practices.